All About The Microbiome
Do you ever look at the millions of stars in the sky and wonder if there's life 'out there'? What you may not realise is that there's a whole universe of life inside your body! Let us take you on a journey deep into your body, to learn about the trillions of life forms that live inside us, known as our 'microbiome'. We'll help you to understand more about how to keep the microbiome healthy and how these microorganisms help to keep their hosts healthy. Read on to find out everything you need to know about the hidden world inside you...
Within this article:
- What is the microbiome?
- The gut microbiome
- The role of the gut microbiome
- The vaginal microbiome
- Dysbiosis: when things go wrong
- The future of the microbiome
- The Microbiome Project
- How to look after your microbiome
What is the microbiome?
I’m sure many of you have watched David Attenborough’s nature shows, which explore different environments such as coral reefs, rainforests, woodlands, or the desert. Each different environment has a unique ecosystem, defined as ‘a community of biological organisms that interact with one another and their physical environment’. A healthy balanced ecosystem benefits both the organisms and the environment.
Just like these other natural ecosystems, the microbiome is a microscopic ecosystem made up of bacteria, yeasts and viruses that live on us, and inside us. That’s right, we are covered in microbes! They live in our mouths, stomach, small intestines, large intestines, urogenital tract, skin, feet, tummy buttons and lungs. Even these different environments encourage different ecosystems. For example, microbes living on the skin tolerate oxygen, whereas gut microbes in the colon can live without oxygen.
The gut microbiome
Generally, when people talk about ‘the microbiome’, they are referring to the gut microbiome, especially those living in the colon (large intestine), as this huge population of microbes is the largest, the most researched, and arguably has the most profound influence over our health. Approximately 40 trillion microbes live on the lining of the small and large intestine (the gut)1 - that’s 5000 times more gut bacteria than people on the planet! Scientists once thought there were more bacteria than human cells in our bodies but the latest advances in technology have suggested a more equal split.
We have evolved with these microbes over thousands of years, forming a symbiotic relationship with them, and passing them on from generation to generation - you likely have similar microbes to your parents, grandparents and great grandparents. But ultimately, your microbiome is completely unique to you. Read on to find out more about the importance of these delicate ecosystems.
The role of the gut microbiome
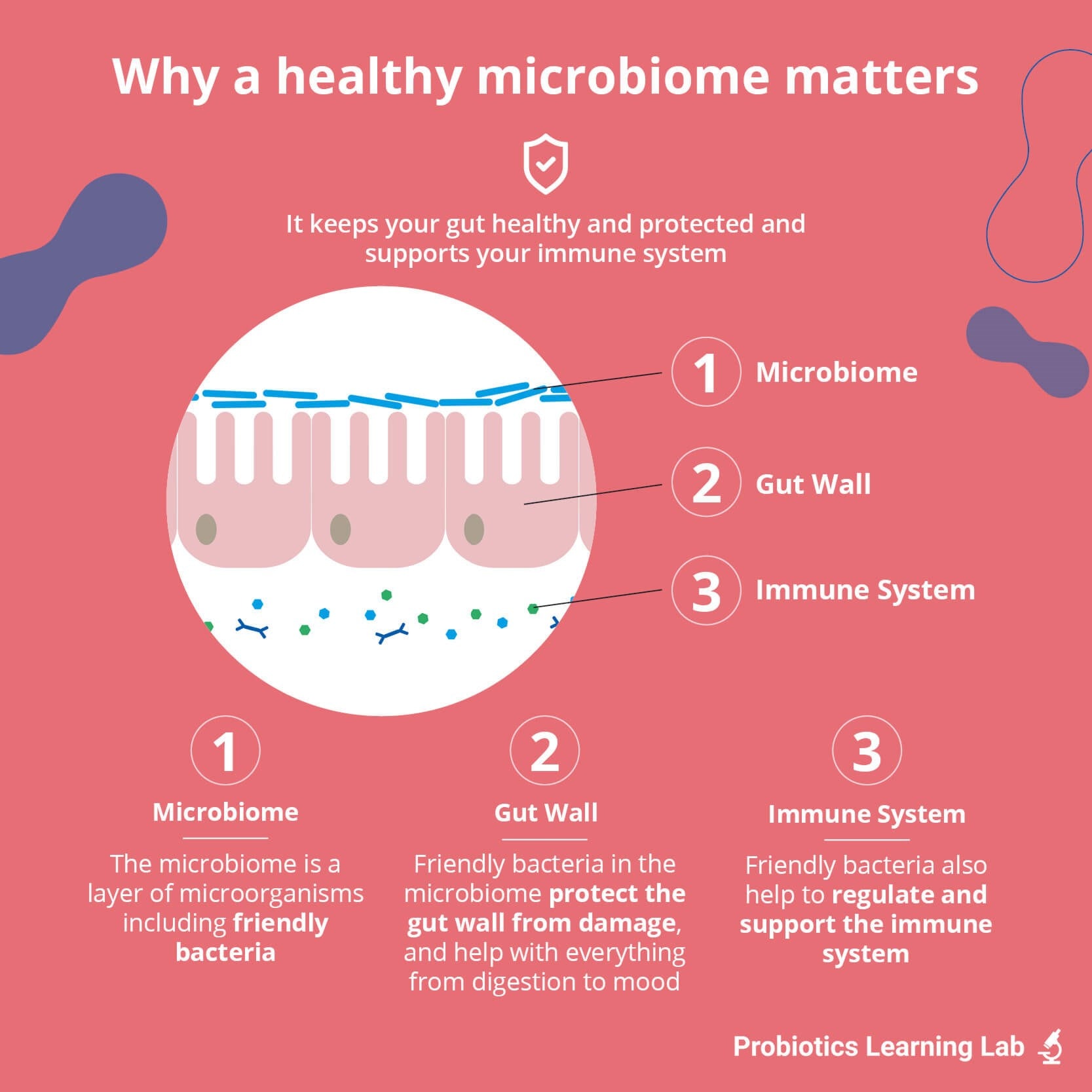
We rely completely on our microbiome. It is estimated that our microbes have 150 times more genes than we do. They carry out essential tasks for us, and our health and wellbeing would be non-existent without them. The list of known functions is already long, but is growing as more and more microbiome research is carried out. Let’s take a look at the role of beneficial gut microbes for our health:
- Digestion: The microbes living in the intestines produce different enzymes (a type of protein) that help us to digest our food. They can help break down lactose and gluten amongst other food sources. When friendly bacteria break down special fibres called prebiotics, they produce beneficial substances that support a healthy gut.
- First-line defence: Imagine it as a line of soldiers with their swords out, ready to defend against invaders. In this case, the bacterial barrier limits harmful bacteria or toxins getting through to the gut cells and immune system.
- Energy levels: Certain strains of bacteria can make B-vitamins, which are known to help with energy levels. Also, as gut bacteria help with digestion, this means we get the maximum energy-boosting nutrients from our food too.
- Immunity: 70% of our immune system is located in the gut, allowing for direct interaction between the microbiota and our immune cells. They go together - what affects one, affects the other. Essentially, the microbiome helps modulate immune responses. Healthcare practitioners can read more about the gut and immunity over on our sister site, Probiotic Professionals.
- Skin health: Friendly bacteria produce beneficial substances in the body, as opposed to the toxins produced by pathogenic (bad) bacteria which can contribute to poor skin.
- Mental health: An emerging area of research is the ‘gut-brain axis’. That’s right - our gut and brain communicate with each other. Many mood-altering neurotransmitters are produced in the gut, including the ‘happy hormone’ serotonin (also a neurotransmitter), so a healthy gut is important for our own happiness. You can find more information on the gut-brain axis here.
The vaginal microbiome
The vaginal microbiome is unique - it’s a completely different environment to the gut. The microbes here have one major job: to reduce the risk of vaginal infections. They create an environment in which friendly bacteria thrive whilst also inhibiting the growth of harmful ones. Find out more about the vaginal microbiome in our dedicated article.
Dysbiosis: when things go wrong
What is the key to a flourishing ecosystem? Balance.
You may have read about the notorious ‘wolves of Yellowstone Park’. The park had high numbers of deer, who had eaten most of the vegetation, leaving little food for other animals. When scientists introduced wolves to the park, they reduced the number of deer and wildlife flooded back - from rabbits, beavers, hawks, bears and fish. The physical environment even changed; the riverbeds got stronger from lack of deer grazing and so the river changed shape.
It’s exactly the same for the microbiome. Whilst all microbes have a role to play in the gut, an overgrowth of harmful microbes is associated with numerous health conditions and they need to be kept in check. A reduced number of friendly bacteria can also result in a weakened intestinal barrier, which can cause a range of problems from digestive issues to allergies. When the gut microbiome is out of balance it is called 'dysbiosis'.

To find out more about dysbiosis and how to address it, you can read Kathy's great article here: ‘What is dybsiosis (and how to address it?)’
The future of the microbiome
Lots of research is being done into the microbiome which will hopefully provide insights into how to manipulate gut bacteria to achieve health benefits. Centres of excellence that are leading the field in this research include Reading University, Cork University and Stanford University.
Most recent research focuses on the link between the microbiome and many areas of our health. Links have been made between dysbiosis in the gut and numerous different health issues. These conditions might be fairly obvious in some cases, but others you may find surprising:
- IBS
- Colic
- Mental health disorders
- Allergies
- IBD, Ulcerative Colitis & Crohn’s disease
- Poor immunity
- Obesity
- Skin disorders: eczema, psoriasis, & acne
- Heart health
- Food intolerances
- Intimate health
- Autism
- Liver disease
- Metabolic syndrome
- Diabetes
- Parkinson’s
What’s really exciting is that research is going even further for a few of these health conditions. Differences in microbial composition can be seen between ‘healthy’ and ‘disease’ states, and as such researchers are looking to develop a ‘microbial algorithm’. The aim of these algorithms is to act as a diagnostic tool and save invasive procedures. This work is in its early days but is promising for the future.
This actually touches on one of the biggest research questions - what came first?
- Dysbiosis and then disease, or
- Disease and then dysbiosis
Either way, it opens up an opportunity to intervene, either by reducing the risk of the disease or managing symptoms.
As Hippocrates stated: ‘all disease begins in the gut'. Wise man!
The Microbiome Project
In 2008, eminent scientists from four different medical centres in the U.S established the Human Microbiome Project, which set out to ‘further our understanding of how the microbiome impacts human health and disease’. The ultimate goal of this project is to establish whether there is a core healthy microbiome seen in the guts of well individuals. It is already known that the exact composition of the intestinal microbiome differs hugely between individuals and that our gut microbiome is said to be as unique to us as our fingerprint.
However, scientists now believe that one-third of the total number of species of bacteria may be common to most people. This opens up the possibility for ‘mapping’ the microbial population and looking for anomalies present in different diseases and health conditions.
It's clear to see that our microbiome plays an enormous role in overall health, and we hope this article has helped you to understand this fascinating system a little bit better.
How to look after your microbiome
You can start with these 3 steps:
- Try incorporating fermented foods or drinks into your diet - these include miso soup, kombucha, kimchi, sauerkraut and kefir. Delicious!
- Watch your sugar intake - sugar feeds the bad bacteria in your gut and can encourage dysbiosis.
- Eat more fibre - fibrous foods are great for your gut health, especially prebiotic fibres, which encourage your body's good bacteria to flourish.
If you want to know more about how to keep your gut healthy, here's a further 10 great tips on looking after your gut microbiome, check out our Gut Health Checklist.
'All about the Microbiome' forms part 1 in our educational resource, ‘Early life microbiome series’, where we introduce you to the microbiome, and take you on a journey through its development and support from conception through to young adulthood. The other articles in this series are:
- All About The Microbiome
- Child Microbiome: Dr Kate's Guide - this explores the factors affecting the microbiome in childhood
- Probiotics for Pregnancy
- Baby Probiotics
- Probiotics for Kids
- Probiotics for Teenagers
You may also be interested in:
What are Probiotics?
How do probiotics work
Gut and Microbiome Health Tests – The Facts
References
- Sender R et al., “Revised Estimates for the Number of Human and Bacteria Cells in the Body,” PLoS ONE, p. 14(8): e1002533., 2016
Popular Articles
View all Gut Health articles-
Gut Health11 Apr 2024
-
Gut Health12 Jan 2024