Probiotics & Bacterial Vaginosis
Bacterial vaginosis (BV) is the most common infection in women of childbearing age, affecting approximately 1 in 3 women. Yet, surprisingly, many women have never even heard of it. In this article, we look at what BV is, how probiotics for BV might help those who are suffering with the condition, and discuss which are the best probiotic strains to use.
- What exactly is bacterial vaginosis?
- What causes BV?
- Which probiotics are best for BV?
- How should you take probiotics for BV?
- Recommendations for long-term BV prevention

What exactly is bacterial vaginosis?
Bacterial vaginosis (BV) is a vaginal condition that creates a grey and watery discharge, which can smell unpleasant. It caused by an overgrowth of bad bacteria, known as pathogens.
In the same way that our gut microbiome is made up of a mixture of ‘friendly’ probiotic bacteria, and a small number of ‘harmful’ pathogenic bacteria, so too is the vaginal microbiome. When pathogens outnumber good bacteria in any microbiome, it is known as dysbiosis, which can lead to infection. You may like to read more about gut dysbiosis and how to address it in the article what is dysbiosis?
If you are diagnosed with BV, it is likely that your doctor will prescribe antibiotics to treat the infection. This may bring temporary relief; however, over time the antibiotics can actually make dysbiosis worse. Read our article about taking probiotics with antibiotics.
BV is usually caused by an overgrowth of Gardnerella vaginalis, though Prevotella, Mycoplasma hominis, and Mobiluncus can also be implicated in BV infections. A healthy vagina contains plenty of bacteria from the Lactobacillus genus. Read this article to find out more about Lactobacillus.
Lactobacilli help to keep the vaginal environment healthy by fermenting glycogen from the vaginal wall to produce lactic acid. Lactic acid decreases the vaginal pH, keeping it within healthy levels below 4.5, which is important for intimate health. If the vagina becomes too alkaline, pathogenic species of bacteria will flourish. This becomes a vicious cycle as pathogenic overgrowth raises the pH, which in turn encourages yet bad bacteria to thrive.
Women are often unaware that they have BV, as in 50% of cases it does not produce symptoms. However, if left untreated it can lead to other complications, such as reduced fertility, increased risk of miscarriage, and reduced birthweights when pregnancy does occur.
What causes BV?
As already explained, BV is an imbalance in the delicate flora which are resident in the vagina. It is not regarded as a sexually transmitted infection.
The vaginal microbiome can become unbalanced for a variety of reasons:
- Sexual activity – whilst BV is not a sexually transmitted infection, having unprotected sex can increase the likelihood of BV infection. This is because each sexual partner may introduce new bacteria into the vagina, disrupting the delicate balance. A 2020 study5 found that oral sex can also disturb the vaginal microbiome. A specific pathogen, Fusobacterium nucleatum, typically found in the mouth and implicated in gum disease, is also associated with BV. It has been found to promote the growth of the most common BV pathogen, Gardnerella vaginalis. The study suggests that the most likely explanation for this pathogen to be found in the vaginal tract is through oral sex.
- If you use an intrauterine device (IUD)
- Smoking
- The use of scented soaps, antiseptic bath liquids or bubble bath or vaginal deodorant – this can alkalise the vagina too much, allowing undesirable strains of bacteria to flourish and infection to occur.
- Douching or flushing the vagina with water or other fluids – this can also alter the pH in the intimate area and encourage the growth of pathogenic bacteria
- The use of strong washing detergents when washing underwear

However, for the large majority of sufferers there is no obvious external cause for the dysbiosis. In these cases, we need to consider the link between the gut flora and the vaginal flora.
Due to the vagina being located close to the anus, it is easy for bacteria to travel from one area to the other. Any pathogenic strains of bacteria that are present in the gut can therefore travel to the vaginal tract via the anus and cause an imbalance of the delicate balance of flora there.
To find out more about how to keep the vaginal microbiome in balance, read this article: All about your vaginal flora.
Which probiotics are best for BV?
Given that BV is an imbalance of bacteria in the vagina, it would make sense that increasing levels of ‘friendly’ bacteria by using probiotic supplements could be beneficial. But which are the best probiotics for bacterial vaginosis?
Scientists are well aware that different probiotics do different things. The probiotic strains which help with BV are able to survive transit through the digestive tract, then migrate to, and colonise, the intimate flora.
It is understood that the Lactobacillus genus is the predominant genus of bacteria found in a healthy vagina, therefore most related research uses strains from the Lactobacillus species. Read this article to find out more about Lactobacillus.
In this section we look at the following Lactobacillus strains which have been researched for the support of BV:
- Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14®
- Lactobacillus paracasei F-19®
- Lactobacillus brevis CD2®, Lactobacillus salivarius FV2®, and Lactobacillus plantarum FV9®
- Lactobacillus acidophilus LA-14® and Lactobacillus rhamnosus HN001
- Lactobacillus crispatus CTV-05
Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14®
In a randomised, double-blind, placebo-controlled study1, 125 women with BV were divided into two groups. One group received a 7-day course of antibiotics, and the second group received both the antibiotics coupled with a probiotic formulation, containing the probiotic strains L. rhamnosus GR-1® and L. reuteri RC-14®. These two strains of friendly bacteria were originally isolated from a healthy vaginal tract, demonstrating that they are a natural and integral part of the vaginal microbiome.
The probiotic supplementation was continued for a further 3 weeks after the end of the antibiotic therapy. Success rates increased from just 40% (as seen with antibiotic therapy alone) to 88% (on the combination therapy)!
Not only do L. rhamnosus GR-1® and L. reuteri RC-14® reach the intimate area and adhere to the vaginal wall lining, they have also been shown to effectively colonise in the intimate area. Their presence in vaginal swabs, taken up to 3 weeks after probiotic supplementation ceased, confirms this.
Health professionals can read more about the research using L. rhamnosus GR-1® and L. reuteri RC-14® on the Probiotics Database.
Key takeaway
- Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14® are natural residents of a healthy vaginal microbiome and have been extensively researched for the support of BV and other vaginal infections.
Lactobacillus paracasei F-19®
A 2006 clinical trial demonstrated that the probiotic strain Lactobacillus paracasei F-19® was able to improve vaginal pH and odour in those with vaginosis5. Women who were orally administered the probiotic Lactobacillus paracasei F-19®, in addition to vaginal suppositories containing Lactobacilllus acidofilus, maintained relief even 3 months after the end of treatment.
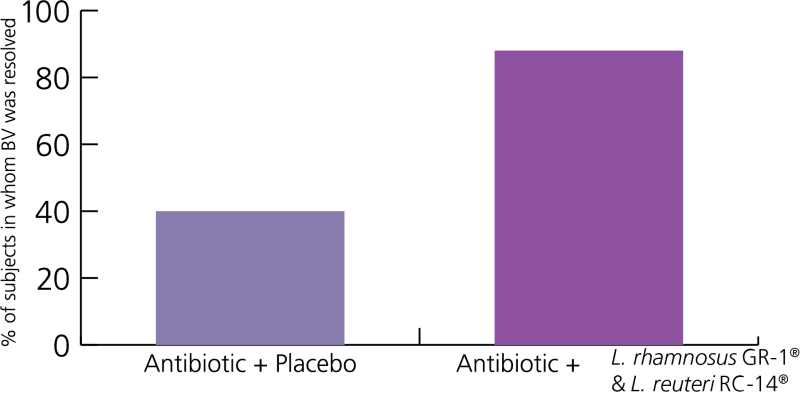
Graph to show efficacy of probiotic strains in supporting those with BV
Another great clinical trial shows further promise for the use of probiotic strains in sufferers of BV. Healthcare practitioners can find out more about this clinical trial on the Probiotic Professionals page.
Key takeaway
- The probiotic strain Lactobacillus paracasei F-19® has been shown to improve vaginal pH and odour in women with BV
Lactobacillus brevis CD2®, Lactobacillus salivarius FV2®, and Lactobacillus plantarum FV9®
In a rather small but well-designed double-blind, randomised, controlled trial2 34 women with BV received either a probiotic tablet or a placebo for 7 days. The probiotic contained at least 10 billion viable Lactobacilli; in particular L. brevis CD2®, L. salivarius FV2®, and L. plantarum FV9®. The 2-week symptom relief rates were 61% (11 out of 18) in the active treatment group. When compared to 19% (three out of 16) in the placebo group (p = 0.017) - these are astounding results!
Key takeaway
- Symptoms of BV have been demonstrated to be relieved by the probiotic strains Lactobacillus brevis CD2®, Lactobacillus salivarius FV2®, and Lactobacillus plantarum FV9®

Lactobacillus acidophilus GLA-14® and Lactobacillus rhamnosus HN001
A double-blind, placebo-controlled randomised trial3 investigated the probiotic strains L. acidophilus La-14® and L. rhamnosus HN001, alongside bovine lactoferrin. When added to antibiotic treatment, this combination was shown to significantly improve symptoms of BV. Furthermore, it also decreased the recurrence rate, as compared with antibiotic treatment alone.
48 adult women presenting with symptoms of BV received either antibiotics and an oral probiotic mixture, plus lactoferrin, for seven days; or antibiotics plus a placebo. Following this, the groups were instructed to take one capsule per day for ten days each month (starting on the first day of menstruation) of either the probiotics plus lactoferrin, or placebo for a duration of six months.
Symptoms such as vaginal discharge and itchiness were markedly improved with the probiotic combination therapy, in comparison to the placebo. Most importantly, recurrence rates were much lower too. Health professionals can visit the Probiotics Database to read more about research featuring L. rhamnosus HN001
Key takeaway
- Lactobacillus acidophilus LA14® and Lactobacillus rhamnosus HN001 probiotic strains have been shown to significantly improve symptoms of BV, when taken in combination with antibiotic treatment
Lactobacillus crispatus CTV-05
Lactobacillus crispatus CTV-05 has recently been assessed in a double-blind randomised placebo-controlled trial for its effects in 228 premenopausal women with recurrent bacterial vaginosis. In the intervention group, women were administered 2 billion CFU of L. crispatus CTV-05 using a vaginal applicator daily for 24 weeks compared with a placebo. By week 12, 30% of the intervention group had a recurrence of bacterial vaginosis compared with 45% of the placebo group (p=0.01). These positive results persisted to week 244.
Key takeaway
- A 2020 trial showed recurrence of BV was lower in premenopausal women taking Lactobacillus crispatus CTV-05
How should you take probiotics for BV?
You might wonder how probiotics work for bacterial vaginosis and whether they are best taken orally or inserted intra-vaginally.
The answer is both methods show the same efficacy, so it depends on individual preference. Most women prefer the ease and convenience of an oral capsule. Research has shown that so long as the correct strains of bacteria are taken orally (i.e. ones that like to colonise in the vaginal tract) then the bacteria are easily able to survive transit through the intestines. They can then make the journey from rectum to vagina. This has been proven in clinical tests whereby the specific probiotics taken have been found in vaginal swabs shortly after they were ingested.
Recommendations for long-term BV prevention
The question regular BV sufferers ask is “how do I prevent BV recurring?”.
We’ve learned so far that BV is an imbalance in the vaginal microbiome, and the following measures may help to keep your intimate flora in balance and reduce your risk of recurring BV infections:
- Following a low sugar diet can be helpful, to reduce the likelihood of glucose being excreted in the urine which can promote an overgrowth of harmful bacteria in the vagina.
- Moderating stress is good for overall health and immunity. A 2018 study7 found a connection between high levels of the stress hormone cortisol and BV. Taking time to relax is important!
- Using unscented, mild bath products and detergents is a good idea as they will not disrupt the normal pH balance of the intimate area.
- Don’t douche or flush the vagina with water - it is designed to be self-cleaning so this is not necessary.
- Using protection during sex can help to prevent pathogenic bacteria being introduced to the vaginal tract and reduces the likelihood of a BV infection
- Consider using an specific probiotic supplement containing highly researched probiotic strains, such as L. rhamnosus GR-1® and L. rhamnosus HN001, which have been shown to help support BV
- Consider supporting gut health too, as we've learned that bad bacteria can translocate from the intestines to the intimate area. Read our article: Gut Health All You Need to Know
If you would like to find out more about female intimate health, you can read more here:
Which probiotics are best for women?
Healthcare practitioners can head over to Probiotics Professionals to find out more about the Lactobacillus genus and its strains on the Probiotics Database.
References
- Anukam, et al. (2006). Augmentation of antimicrobial therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 andLactobacillus reuteri RC-14. Microbes Infect, 8(6): pp. 1450-4
- Mastromarino et al. (2009). Effectiveness of Lactobacillus-containing vaginal tablets in the treatment of symptomatic bacterial vaginosis. Clin Microbiol Infect, 15(1): pp. 67-74
- Russo R et al. (2018). Evidence-based mixture containing Lactobacillus strains and lactoferrin to prevent recurrent bacterial vaginosis: a double blind, placebo controlled, randomised clinical trial. Beneficial Microbes, Published online ahead of print on December 10, 2018.
- Cohen, C. et al. (2020) "Randomized Trial of Lactin-V to Prevent Recurrence of Bacterial Vaginosis," The New England Journal of Medicine , pp. 382 (20), 1906-1915
- Delia A, et al., 2006
- Agarwal K. 2020. Glycan cross-feeding supports mutualism between Fusobacterium and the vaginal microbiota. PLOS Biology. https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3000788
- Amabebe E, Anuma D (2018) Psychosocial Stress, Cortisol Levels, and Maintenance of Vaginal Health. Frontiers in Endocrinology, 9: 568
Popular Articles
View all Women's Health articles-
Women's Health13 Feb 2024
-
Women's Health12 Jan 2024
-
General Health31 Oct 2023


