Which probiotics help with thrush?
Thrush is a very common health issue which affects 130 million women worldwide every year1. It can be a source of discomfort and frustration for many women. As such, more individuals are looking for natural options to help manage their symptoms and prevent recurrent infection. Probiotics have become a popular option. However, identifying the right probiotic to help combat thrush is important as some are much more effective than others. Find out more about the best strains for female intimate health in this article on our Probiotics Learning Lab 'Which Probiotics are best for Women?'
Some of the most well researched probiotics for yeast infections, specifically shown to help with thrush in clinical trials, are Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1®. These interesting strains are discussed in detail below.
In this article we will look at:
- What is thrush?
- What are the causes of thrush?
- Can probiotics help with thrush?
- Does live yoghurt help with thrush?
- How do probiotic supplements help prevent thrush?
- Which is the best probiotic for thrush?
- Reducing the risk of thrush
- Can men get genital thrush?
- Oral thrush
- Summary
What is thrush?
Thrush is a yeast infection caused by a pathogenic (harmful) yeast. This can occur in the mouth (oral thrush) or in the genital area (vulvo-vaginal thrush). The typical symptoms of vaginal thrush include:
- Vaginal discharge - creamy white, “cottage cheese -like”, usually odourless
- Itching and irritation of the intimate area affecting the labia and entrance to the vagina
- Severe cases – skin breakdown and excoriation
- Other potential additional symptoms – pain during intercourse, discomfort/burning when urinating, sometimes asymptomatic
Women can often suffer with multiple bouts of thrush, the recurrence rates are quite high with a prevalence of 9% of women suffering between the ages of 25 to 34 years globally1. Traditional medical treatment involves the use of topical anti-fungal creams, anti-fungal pessaries or oral anti-fungal tablets. However, extensive use of these is contributing negatively to an already increasing rate of anti-fungal resistance in Candida spp2.

What are the causes of thrush?
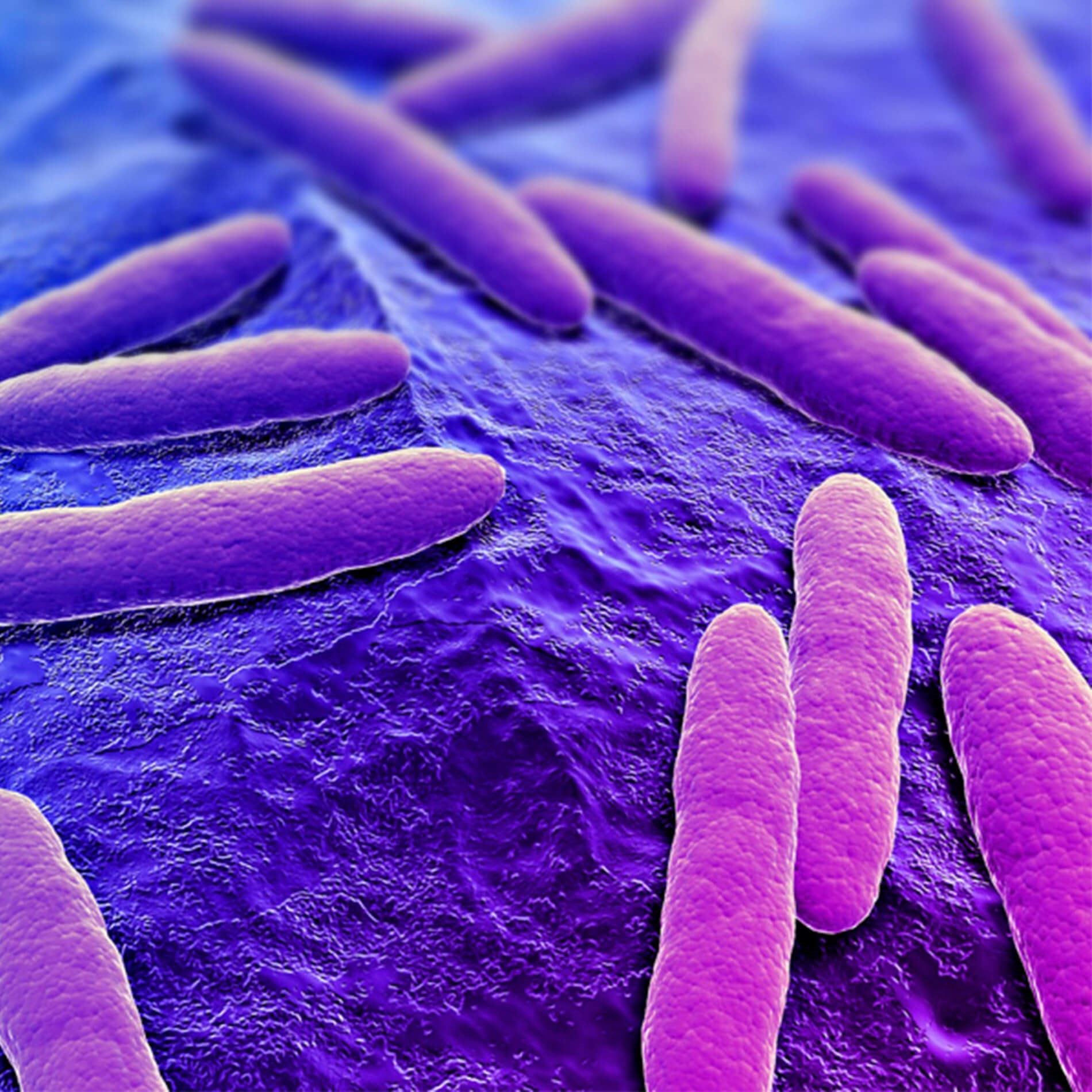
Thrush is typically caused by a pathogenic yeast known as Candida. Candida spp. lives naturally in the body - within the intestines, mouth, skin and vagina. In low numbers, they are usually considered harmless. The most common species of Candida that can cause thrush is Candida albicans.
Candida albicans (C. albicans) may increase in number when there is an imbalance, known as dysbiosis, in the microbiome. The human microbiome is the name given to the microbes that live on or within the human body including bacteria and yeasts. Collectively, they form an ecosystem. There is usually a delicate balance between the beneficial microbes and pathogenic microbes in our microbiome. Symptoms of thrush may develop when there is an overgrowth of C. albicans in the mouth or genital area. This overgrowth is believed to occur as a result of a disruption to our microbiome, leading to dysbiosis. This disruption may occur due to factors such as:
- Medication use - antibiotics, oral contraceptive pill3 or hormonal replacement therapy4, corticosteroids5
- Fluctuations in hormone levels such as during pregnancy3 Disruption of the natural pH balance of the vagina caused by local factors such as use of scented intimate products and soaps.
- Underlying medical conditions such as Diabetes Mellitus6
- Dietary habits – excessive alcohol consumption, high sugar/low fibre diets
- Sexual activity7
The vaginal microbiome is unique and differs from the oral and gut microbiome. A healthy vaginal microbiome should be dominant in the bacteria, lactobacilli. Lactobacilli can exert many protective effects to promote a healthy vaginal tract and reduce the risk of infections. When their levels are depleted, an imbalance may occur and opportunistic pathogens such as C. albicans can thrive.
Can probiotics help with thrush?
Yes, probiotics may help with managing thrush and yeast infections. Clinical studies have shown that optimising one's friendly bacteria with probiotics can help to maintain a healthy vaginal microbiome. However, probiotics work in different ways - many work predominately in the gut. Not all lactobacilli will even reach the vaginal tract. It’s important to find probiotic strains that have evidence for vaginal colonisation and have clinical trials against thrush.
Which is the best probiotic for thrush?
A number of clinical trials testing a combination of two particular probiotic strains, Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1® have been shown to be hugely beneficial in supporting those suffering from yeast infections. The best probiotic for yeast infections include the two strains of bacteria, L. reuteri RC-14® and L. rhamnosus GR-1®, which are some of the most researched probiotics to date, and are certainly the most researched in terms of women's intimate health. You may like to read about further research behind these two strains on the Probiotics Database behind Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1®
In a RCT by Martinez et al. 2009, 55 women diagnosed with vulvovaginal candidiasis were divided into two groups; one group received 2 billion CFU of Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1® and the other group received a placebo for 4 weeks. Both groups initially were given 150mg of oral fluconazole. There was a significant reduction in vaginal discharge which corresponded with a reduction in yeast cell counts on vaginal swabs. More subjects with recurrent infection tested positive for Candida spp. on vaginal swabs compared with the probiotic group at the end of the 4 weeks (80% and 18.2% respectively)8. This shows that use of these two strains of probiotic bacteria alongside conventional oral anti-fungal medication, can enhance the efficacy of the antifungal medication. This is particularly relevant for individuals who suffer with vaginal thrush recurrently despite use of conventional treatments. In further studies by Anukam et al. 2009, oral supplementation with these two strains alongside conventional treatment resulted in reduced recurrence of future infections9.
Does live yoghurt help with thrush?
Live yoghurts are a good source of friendly bacteria. It is beneficial to consume probiotic foods, such as live yoghurt, to boost our overall general health. Keeping our gut microbiome healthy by eating live yoghurt, will in turn help our vaginal microbiome, and help avoid an imbalance that could lead to thrush. However, the probiotic bacteria that are present in live yoghurt are not specific for vaginal health, and may not even reach the intimate area. Using a probiotic supplement that has been clinically researched for supporting vaginal health, may provide a much more targeted approach when managing thrush and yeast infections.
How do probiotic supplements help prevent thrush?
Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1® have been shown to have anti-fungal properties. Both strains can produce lactic acid, this helps to lower the pH in the vaginal tract (pH 4 or below). This acidity creates an unfavourable environment for C. albicans, thus limiting growth. The probiotic strains can also adhere to the vaginal lining and create a physical barrier limiting the space and nutrients available for C. albicans (known as competitive inhibition)10. Furthermore, both strains may reduce inflammation associated with C. albicans infection. These strains inhibited the growth of Candida albicans through the production of anti-fungal, lactic acid and competitive inhibition, by utilising space and nutrients Candida albicans requires to grow .
Reducing the risk of thrush
Other lifestyle factors may need to be considered when managing or reducing the risk of thrush
Try to avoid:
- Tight-fitting underwear and tights
- Perfumed soaps and shower gels including products marketed specifically for the vagina
- Alcohol and high sugar foods.
Choose:
- A good quality probiotic specifically researched for women’s intimate health
- Cotton underwear rather than synthetic materials
- To wash the intimate area with water alone or with a clean, wet cloth
Can men get genital thrush?
Although less common, it is possible for men to get thrush. The cause of thrush in men is usually an overgrowth of the yeast-like fungus, Candida albicans. Symptoms include itching, burning, irritation and redness of the penis. Currently, there are no genital probiotics which are studied for thrush in men, however, men with thrush could consider supporting their gut health. Our article 'Which probiotics are best for Candida?' can provide helpful tips and guidance on how to do this.
Oral thrush
The above information relates predominantly to vaginal thrush. More scientific research is needed but preliminary studies do support the theory that probiotics for thrush could also have a role to play in the management of oral thrush. As a health care professional you might find the following blog post interesting: Could probiotics help with oral thrush?
Summary
- Vulvovaginal thrush is caused by an overgrowth of Candida, most commonly Candida albicans.
- Due to high recurrence rates, women are seeking alternative options to traditional treatments, to help manage their symptoms.
- Supporting a healthy vaginal microbiome can help to correct imbalance of Candida spp. overgrowth.
- Identifying a probiotic that reaches the vaginal tract and has clinical evidence against thrush in particular is important.
- A healthy vaginal microbiome which is high in lactobacilli may protect against gynaecological infections such as thrush.
- The best probiotics for yeast infections like thrush include the strains Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1® which have promising clinical research for their role in supporting vaginal health.
References
- Denning, D. W., Kneale, M., Sobel, J. D., & Rautemaa-Richardson, R. (2018). Global burden of recurrent vulvovaginal candidiasis: a systematic review. Lancet Infect Dis, 339-347.
- Berkow, E. L., & Lockhart, S. R. (2017). Fluconazole resistance in Candida species: a current perspective. Infection and Drug Resistance, 237-245.
- Jacob, L., John, M., Kalder, M., & Kostev, K. (2018). Prevalence of vulvovaginal candidiasis in gynecological practices in Germany: A retrospective study of 954,186 patients. Current Medical Mycology, 6-11.
- Fischer, G., & Bradford, J. (2011). Vulvovaginal Candidiasis in postmenopausal women: the role of hormonal replacement therapy. Journal of Lower Genital Tract Disease, 263-267.
- Farhan, M. A., Moharram, A. M., Salah, T., & Shaaban, O. M. (2019). Types of yeasts that cause vulvovaginal candidiasis in chronic users of corticosteroids. Medical Mycology, 681-687.
- Rodrigues, C. F., Rodrigues, M. E., & Henriques, M. (2019). Candida spp. Infections in Patients with Diabetes Mellitus. Journal of Clinical Medicine.
- Foxman, J. (1990). The Epidemiology of Vulvovaginal Candidiasis: Risk Factors. American Journal of Public Health.
- Martinez et al., (2009), ‘Improved treatment of vulvovaginal candidiasis with fluconazole plus probiotic Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14®’. Lett. Appl. Microbiol., 48(3): 269-74.
- Anukam et al., (2009), ‘Oral use of probiotics as an adjunctive therapy to fluconazole in the treatment of yeast vaginitis: A study of Nigerian women in an outdoor clinic’. Microb. Ecol. Health Dis., 21(2):72-77.
- Kohler, G. A., Asseifa, S., & Reid, G. (2012). Probiotic Interference of Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 with the Opportunistic Fungal Pathogen Candida albicans. Infectious Diseases in Obstetrics and Gynaecology.
This article was written by Dr Aisling Dwyer MB BCh BAO (Medicine, Surgery and Obstetrics), MSc (Personalised Nutrition) in collaboration with Kathy Wheddon (Nutritional Therapist DipION).