Gut-Brain Axis and Probiotics
What is the Gut-Brain Axis?
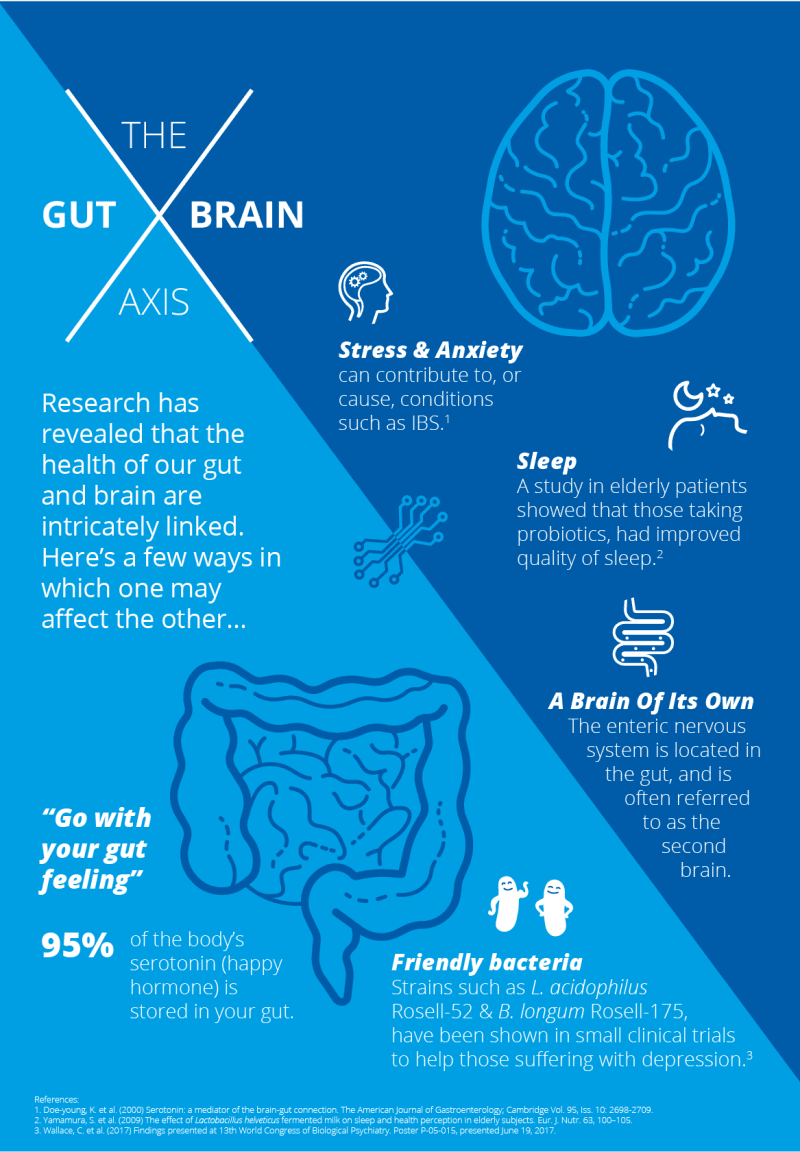
The Gut-Brain Axis is currently a hot topic, but the idea of a gut-brain connection is nothing new: ‘Go with your gut feeling’ is a very old saying. Over the past ten years, however, this old adage is being supported by the results of hundreds of scientific studies exploring the potential of this fascinating subject.
Unfortunately, mental health issues are rapidly on the rise and a 2021 study showed that during the COVID-19 pandemic, about 4 in 10 adults in the U.S. reported symptoms of anxiety or depressive disorder, up from 1 in 10 adults who reported these symptoms from January to June 20191. Multiple studies on the U.K. population reveal deteriorations in mental health during the pandemic with fluctuations of improvement but not to pre-pandemic levels2. Sadly, the largest increase in both countries was seen amongst those aged 18–29; meaning it is more important now than ever to understand how the gut microbiome interacts with the brain, and how nutritional interventions including specific diets and the use of pre and probiotics (together referred to as synbiotics) can act as a therapeutic tool in dealing with mental health disorders3.
Read on to find out more about the gut-brain connection, or jump to the topic that interests you the most:
- The physical connection between gut and brain
- What is the microbiome gut-brain axis?
- Gut microbiome and mental health
- ‘Psychobiotics’ – the anti-depressants of the future?
- Does our unique microbiota influence our personality?
The physical connection between gut and brain
We now understand that the gut and the brain are connected, but how do these two remote areas of the body interact? In physical terms, the brain is connected to the digestive system by the vagus nerve, the longest of twelve different cranial nerves linking our intestinal nervous system to the central nervous system (CNS). This vital part of the neural network controls and coordinates a variety of key but ‘unconscious’ bodily functions from our heart rate to the digestive process.
Most view our digestive system as a reasonably simple pipe through which our food and drink pass, when in fact the intestinal tract has its own highly complex nervous system, known as the 'enteric or intrinsic nervous system' (Glossary definition: enteric or intrinsic nervous system) connected to the CNS via the vagus nerve. Because the intestines host such a multitude of neurons, scientists have re-christened the gut ‘the second brain’4.
What is the microbiome gut brain axis?
Now we’ve learned about the physical connection between the gut and the brain, what part do our gut bacteria play in this relationship?
Studies suggest that microbes in the gut actually release chemical messengers that influence cell responses along the vagus nerve – acting just like our body cells – and send communications via the vagus nerve to the brain.4,9 The gut bacteria provide the (bio)'chemistry' that binds this couple together!
A new study demonstrates the gut microbiome of patients with social anxiety disorder (SAD) differs in composition and function to that of healthy controls, suggesting that the microbiome-gut-brain axis may represent a potential therapeutic target for this chronic disorder10.
Gut microbiome and mental health
In terms of the gut microbiome and mental health, the most obvious connection is the ‘fight or flight’ response which sends us running to the loo in stressful situations, but scientists are now recognising that may be far broader implications for health.
Neuroscientists are establishing a role for the gut microbiota in many mental health disorders from Parkinson’s disease to depression, while other studies have investigated the potential of probiotics in the support of social anxiety and other related conditions. Health professionals can read about probiotics for stress and anxiety over at our sister site: Probiotics Professionals.
Altered gut microbiota and digestive issues are often noted in children with Autism Spectrum Disorders (ASD), and it is believed the gut-brain connection could have a significant role in the development of the condition and the behaviour of those affected5.
Recent research has also highlighted a potential link between the gut and brain in people with bipolar disorder (BD). The study found that gut microbiota composition is different in BD patients compared with the control group. Those with bipolar disorder tended to have a greater abundance of Bacilli and Lactobacillales genus, which researchers found to be correlated to a greater severity of depression11.
What is depression?
Depression is by far one of the most common mental disorders in modern society, and millions of people worldwide suffer from a broad range of syndromes falling under the term ‘depressive disorders’.
This term encompasses a variety of conditions from social anxiety to seasonal affective disorder and is linked to other mental health disorders such as ‘OCD’ (obsessive compulsive disorder) and PTSD (post-traumatic stress disorder).
‘Psychobiotics’ – the anti-depressants of the future?

Could future mental disorders be helped by manipulating the gut microbiome? Will gut-brain probiotics be used as a natural first line intervention alongside, or even instead of, anti-depressants?
Specific studies have looked at the possibility of applying probiotic bacteria to help alleviate symptoms of depression12. The term 'psychobiotics’ was coined in 2013 by two scientists and describes a live organism that, when ingested in adequate amounts, produces a health benefit in patients suffering from psychiatric illness.
A study published in the journal ‘Nutrition’ looked at the effects of probiotic supplementation on a group of subjects known to be suffering from Major Depressive Disorder. Forty participants aged between 20 and 55 years old were separated into two groups: one group was given a probiotic supplement containing three species of bacteria, Lactobacillus acidophilus (2 × 109 CFU/g), Lactobacillus casei (2 × 109 CFU/g), and Bifidobacterium bifidum (2 × 109 CFU/g), and the other group was given a placebo. Their diets were also assessed along with their exercise regimes.
After an eight week period, the group given the probiotics saw significant and measurable improvements on their Beck Depression Inventory, insulin, homeostasis model and assessment of insulin resistance6. You can read more about this concept in our blog: ‘Psychobiotics – just a fad? Or here to stay?'.
Don’t forget diet
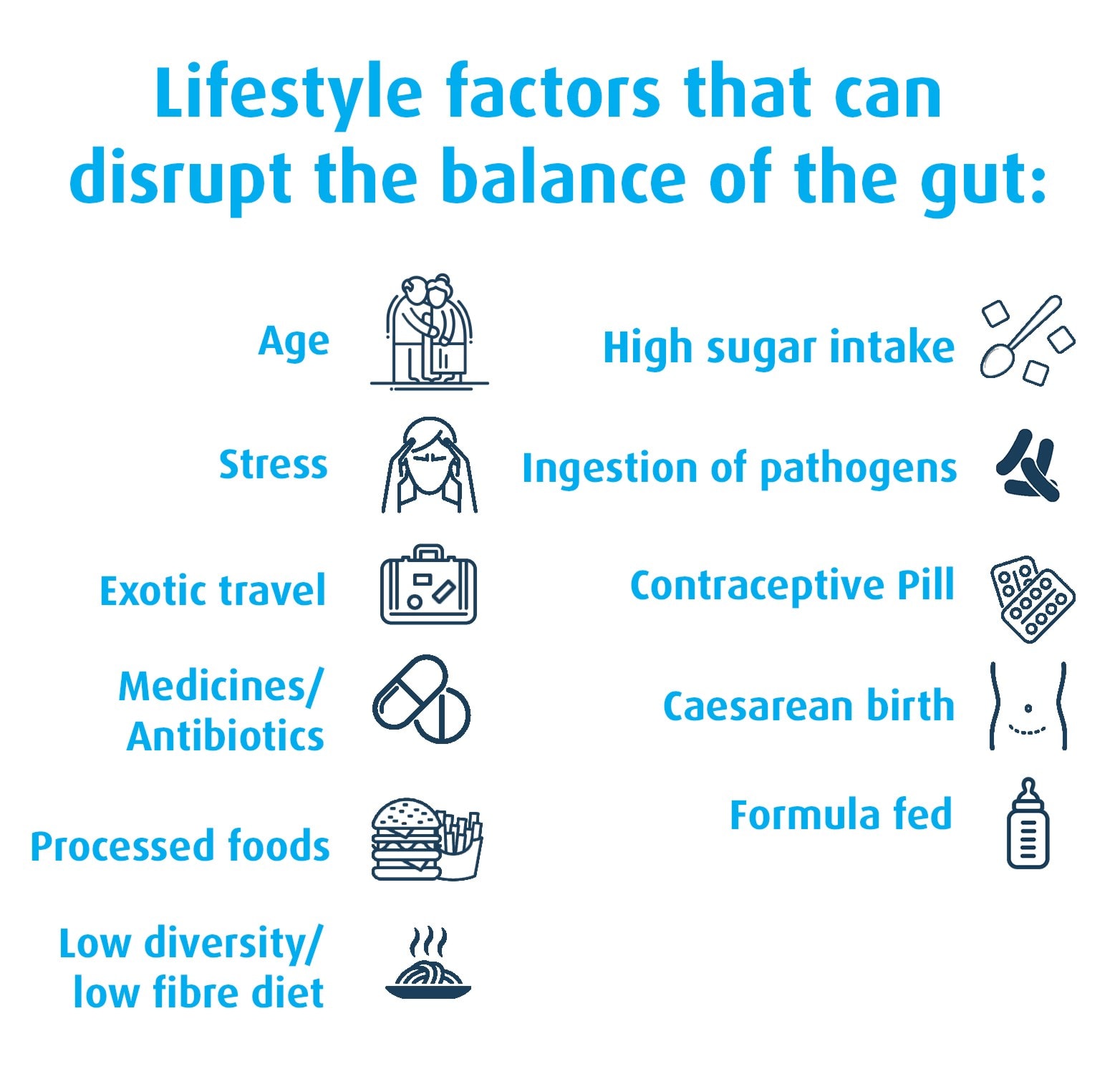
Our diet can also significantly affect our mental health - the food we eat directly influences the type of microflora that flourish in our intestines15. Dr. Perlmutter, president of the Perlmutter Brain Foundation, recommends that a diet rich in fermented foods and good bacteria is key to good brain health, and suggests a diet plan in his book, 'Brain Maker'.
Professor Tim Spector from King’s College London conducted an experiment assessing the effects of junk food on the microbiome of his son, Tim junior. Prior to the experiment, young Tim’s gut microflora contained over 3,500 different species of bacteria, but after ten days these populations had plummeted down to just 1,300 species. Wipe-out!
There has also been research into Vitamin D for SAD (seasonal affective disorder), a more severe version of the 'winter blues'. SAD is a seasonal type of depression, typically occuring in the darker winter months. Because of the links between Vitamin D for gut health and SAD, probiotics can be a way to positively alter the gut microbiome and help aleviate symptoms of low mood and depression13,14.
Does our unique microbiota influence our personality?
Do tantrums begin in the tum? Do certain types of bacteria affect our behaviour and memory? Should future psychological profiling tests include a breakdown of our gut microbiota?
Studies suggest that pathogenic bacteria make us crave sugary foods7 and a recent study indicated that gut bacteria significantly affected the mood of toddlers. The research at Ohio State University focused on the spectrum of bacteria extracted from the intestines of a group of children.
The study was originally focused on the role of gut bacteria in the development of future health issues such as obesity, asthma, allergies and bowel disease. But whilst looking for clues as to how these toddlers’ microbiome might influence their adult health, the researchers noted that the presence of certain types of bacteria, the diversity of species and the size of the bacterial populations noticeably affected the behaviour of the children.8,9 Fascinating stuff!
A marriage made of gut health and mental health
If you are trying to support mental health symptoms, then it appears that the key to our overall state of our sense of well-being lies in ensuring that there is a healthy relationship between our gut and our brain.
Two strains that have shown promise in this emerging field of 'psychobiotics' are Lactobacillus acidophilus Rosell-52 and Bifidobacterium longum Rosell-175. You can read more about them in the article: 'Probiotics for stress'.
Healthcare Professionals can also learn more about the strains on the Probiotics Database: Lactobacillus acidophilus Rosell-52
New to probiotics and gut health? Find out more:
Gut Health - All You Need to know
The Microbiome & Emotional Health
References
- Anjel Vahratian, Stephen J. Blumberg, Emily P. Terlizzi, Jeannine S. Schiller. (2021). Symptoms of Anxiety or Depressive Disorder and Use of Mental Health Care Among Adults During the COVID-19 Pandemic — United States, August 2020–February 2021. MMWR Morb Mortal Wkly Rep. 70 (13), 490–494.
- GOV.UK. (2021). COVID-19 mental health and wellbeing surveillance: report. Available: https://www.gov.uk/government/publications/covid-19-mental-health-and-wellbeing-surveillance-report/2-important-findings-so-far. Last accessed 16th December 2021.
- Muhammad Naveeda, Qi-Gang Zhoub, Chu Xub, Abdoh Taleba, Fan Mengb, Bilal Ahmeda, Yu Zhanga, Kohji Fukunagac, Feng Hana. (2021). Gut-brain axis: A matter of concern in neuropsychiatric disorders…!. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 104 (1), 1-10.
- Perlmutter, R. (2015) ‘Brain Maker’: Hodder & Stoughton: London
- Krajmalnik-Brown et al, (2015) , ‘Gut bacteria in children with autism spectrum disorders: challenges and promise of studying how a complex community influences a complex disease’, Microbial Ecology in Health and Disease, Vol 26 (2015).
- Akkasheh et al, (2015) ‘Clinical and metabolic response to probiotic administration in patients with major depressive disorder: A randomized, double-blind, placebo-controlled trial’, Nutrition, September 25, 2015
- Lisa M. Christian, et al (2015), Gut microbiome composition is associated with temperament during early childhood. Brain, Behavior, and Immunity, 2015; 45: 118 D
- Ohio State University Center for Clinical and Translational Science. "Toddler temperament could be influenced by different types of gut bacteria." ScienceDaily. ScienceDaily, 27 May 2015. www.sciencedaily.com/releases/2015/05/150527091438.htm>.OI:10.1016/j.bbi.2014.10.018
- William W.L. Hsiao, et al (2008), The Microbes of the Intestine: An Introduction to Their Metabolic and Signaling Capabilities. Endocrinol Metab Clin North Am. 2008 Dec; 37(4): 857–871.doi: 10.1016/j.ecl.2008.08.006
- Butler MI et al., (2023) The gut microbiome in social anxiety disorder: evidence of altered composition and function, Translational Psychiatry, 13, Article number: 95
- Huang T etal., (2023) Gut microbiota and its relation to inflammation in patients with bipolar depression: a cross-sectional study. Annals of General Psychiatry, 22:21.
- Zhang Q et al., (2023) Effect of prebiotics, probiotics, synbiotics on depression: results from a meta-analysis. BMC Psychiatry, 23:477.
- Luna RA, Foster JA. Gut brain axis: diet microbiota interactions and implications for modulation of anxiety and depression. Curr Opin Biotechnol. 2015;32:35-41.
- O’Mahony SM, Clarke G, Borre YE, Dinan TG, Cryan JF. Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behav Brain Res. 2015;277:32-48.
- Ke, S., Wang, XW., Ratanatharathorn, A. et al. Association of probable post-traumatic stress disorder with dietary pattern and gut microbiome in a cohort of women. Nat. Mental Health 1, 900–913 (2023). https://doi.org/10.1038/s44220-023-00145-6
Popular Articles
View all Mental Health articles-
Mental Health22 Nov 2023
-
Mental Health05 Jan 2024
-
Women's Health12 Jan 2024


